Fill Out a Valid Tb Test Template
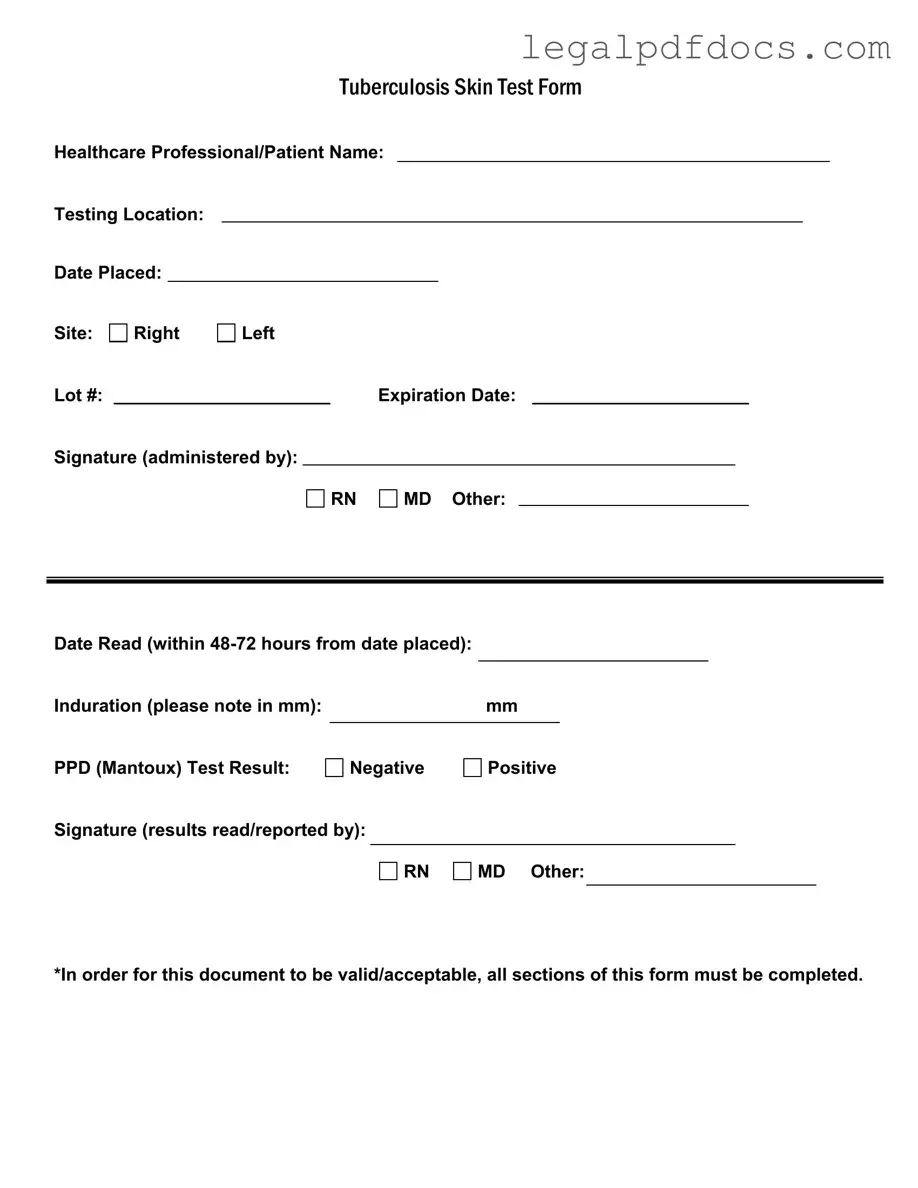
The Tuberculosis (TB) Skin Test form is an essential document used in the assessment of TB exposure and infection. This form captures critical information related to the testing process, including the names of both the healthcare professional and the patient, as well as the location where the test was administered. It also records the date the test was placed and the specific site on the body where the test was conducted, indicating whether it was on the right or left arm. Each test is assigned a unique lot number, along with an expiration date to ensure the validity of the test materials used. The signature of the administering professional—be it a registered nurse (RN), medical doctor (MD), or another qualified individual—confirms the test's administration. After a specified period of 48 to 72 hours, the results are read, and the induration, or swelling, is measured in millimeters (mm), which is crucial for determining the outcome. The form concludes with the test result, indicating whether the PPD (Purified Protein Derivative) test is negative or positive, and requires the signature of the professional who reported the results. To maintain its validity, it is imperative that all sections of this form are thoroughly completed.
Dos and Don'ts
When filling out the TB Test form, it's essential to be thorough and accurate. Here are some helpful dos and don'ts to guide you through the process.
- Do provide your full name and the name of the healthcare professional administering the test.
- Do clearly indicate the testing location and the date the test was placed.
- Do specify the site of the test, whether it’s the right or left arm.
- Do ensure that the lot number and expiration date of the test are filled out correctly.
- Do sign the form to confirm that the test was administered.
- Don't leave any sections blank; all parts of the form must be completed for it to be valid.
- Don't forget to record the date when the test results will be read, which should be within 48-72 hours.
- Don't neglect to measure and note the induration in millimeters accurately.
- Don't skip the signature section for the results; it’s crucial for documentation.
By following these guidelines, you can help ensure that your TB Test form is completed correctly and efficiently. This not only aids in your health assessment but also streamlines the process for healthcare professionals.
How to Use Tb Test
Filling out the TB Test form is a straightforward process, but it requires attention to detail to ensure that all necessary information is accurately recorded. After completing the form, the next steps typically involve submitting it to the appropriate healthcare professional or institution for review and record-keeping.
- Start by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being administered.
- Record the Date Placed—the date when the test is given.
- Indicate the Site of the test, marking either Right or Left.
- Enter the Lot # of the test used.
- Fill in the Expiration Date of the test.
- Provide the Signature of the person administering the test, selecting from RN, MD, or Other.
- Record the Date Read—this should be within 48-72 hours from the date placed.
- Measure and note the Induration in millimeters (mm).
- Document the PPD (Mantoux) Test Result as either Negative or Positive.
- Lastly, have the Signature of the person who read or reported the results, again selecting from RN, MD, or Other.
Make sure that all sections of the form are completed to ensure its validity and acceptance.
More PDF Templates
S Corp Abbreviation - The form is a critical element in establishing a corporation’s desired tax classification with the IRS.
Citi Bank Direct Deposit - Direct deposit means no more trips to the bank—just fill out this form.
Immunization Records Florida - This document stands as a testament to collective efforts in disease prevention and public health stabilization.
Documents used along the form
The Tuberculosis (TB) Test form is an essential document used to record the results of a TB skin test. However, it often accompanies other forms and documents that help provide a complete picture of a patient's health status and testing history. Here are five other commonly used forms and documents related to TB testing.
- Patient Health History Form: This document collects information about a patient's medical history, including previous illnesses, vaccinations, and any known allergies. It helps healthcare providers understand the patient's overall health and any risk factors for TB.
- Consent Form: Before administering the TB test, patients are often required to sign a consent form. This document ensures that patients are informed about the procedure, its purpose, and any potential risks involved.
- Follow-Up Evaluation Form: If a TB test result is positive, a follow-up evaluation form may be used to document further assessments. This includes chest X-rays or additional tests to determine if the patient has active TB disease.
- Vaccination Records: This document outlines a patient’s vaccination history, including the BCG vaccine, which is sometimes given in countries with high TB rates. It helps healthcare providers assess the patient's immunity and risk for TB.
- Referral Form: If a patient needs specialized care following a positive TB test, a referral form is used to direct them to a specialist. This ensures that the patient receives the appropriate follow-up care and treatment.
In summary, these documents work together with the TB Test form to provide a comprehensive understanding of a patient's health regarding tuberculosis. Properly completing and managing these forms is crucial for effective patient care and disease management.
Misconceptions
Understanding the Tuberculosis (TB) Test form is crucial for both healthcare professionals and patients. However, several misconceptions can lead to confusion. Here are six common misunderstandings about the TB Test form:
- All sections of the form are optional. Many believe that some sections of the TB Test form can be left blank. In reality, every section must be completed for the document to be valid and acceptable.
- Only a doctor can administer the test. While it is true that a doctor can administer the test, other qualified healthcare professionals, such as registered nurses (RNs), can also perform this task.
- The test result is immediate. Some individuals expect to receive their test results right after the test is administered. However, the results are typically read within 48 to 72 hours after placement.
- A negative result means no exposure to TB. A negative result indicates that there is no current infection; however, it does not completely rule out past exposure to the bacteria that cause TB.
- Induration measurement is not important. Many overlook the significance of the induration measurement in millimeters. This measurement is crucial for interpreting the results of the PPD (Mantoux) test.
- Expiration dates are not relevant. Some may disregard the expiration date listed on the form. It is important to ensure that the test materials are within their expiration date to guarantee accurate results.
File Specs
| Fact Name | Description |
|---|---|
| Form Title | This form is officially titled "Tuberculosis Skin Test Form." |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test. |
| Testing Location | The specific location where the test is administered must be recorded. |
| Date Placed | The date when the test is administered needs to be noted on the form. |
| Site of Test | The form includes a section to indicate whether the test was placed on the right or left arm. |
| Lot Number | A lot number for the PPD solution must be documented for traceability. |
| Expiration Date | The expiration date of the PPD solution is required to ensure validity. |
| Date Read | The results must be read and recorded within 48 to 72 hours of administration. |
| Induration Measurement | The induration, if present, must be measured in millimeters and noted on the form. |
| Test Result | The result of the PPD (Mantoux) test must be clearly indicated as negative or positive. |
Key takeaways
When filling out and using the TB Test form, it is essential to pay attention to several key aspects to ensure accuracy and compliance. Here are the main takeaways:
- Complete All Sections: Ensure that every section of the form is filled out. Incomplete forms may not be accepted.
- Accurate Information: Provide correct details for the healthcare professional and patient, including names and testing location.
- Date Management: Note the date the test is placed and the date it is read. The results must be recorded within 48-72 hours.
- Induration Measurement: Measure the induration accurately in millimeters (mm) and record this information clearly.
- Result Documentation: Clearly indicate whether the PPD (Mantoux) test result is negative or positive.
- Signature Requirement: Ensure that the administering professional signs the form, along with the individual reading the results.
- Expiration Awareness: Check the expiration date of the lot number used for the test to ensure validity.