Official Do Not Resuscitate Order Form for Michigan
In Michigan, the Do Not Resuscitate (DNR) Order form serves as an essential tool for individuals who wish to make their healthcare preferences known regarding life-sustaining treatments. This form is particularly important for those facing serious medical conditions or end-of-life decisions. By filling out the DNR Order, patients can clearly communicate their desire to forgo cardiopulmonary resuscitation (CPR) and other aggressive measures in the event of a cardiac arrest or respiratory failure. The form must be signed by both the patient and their physician, ensuring that the decision is informed and supported by medical guidance. It is also vital to understand that this order applies in emergency situations, guiding first responders and healthcare providers in respecting the patient's wishes. The DNR Order is not a blanket refusal of all medical care; rather, it specifically addresses the use of resuscitative efforts, allowing for other forms of treatment to continue. Understanding the nuances of this form can empower individuals to take control of their healthcare decisions and ensure that their preferences are honored, even in critical moments.
Dos and Don'ts
When filling out the Michigan Do Not Resuscitate Order form, it is important to approach the process with care. Here are some things you should and shouldn't do:
- Do ensure that you fully understand the implications of a Do Not Resuscitate Order.
- Do discuss your wishes with your healthcare provider and family members.
- Do fill out the form clearly and legibly to avoid any confusion.
- Do keep a copy of the completed form in a safe place and share it with your healthcare team.
- Don't sign the form without discussing it with your doctor.
- Don't forget to update the form if your wishes change.
- Don't assume that verbal instructions are enough; always use the official form.
Taking these steps can help ensure that your wishes are respected and understood. Your health and peace of mind are important.
How to Use Michigan Do Not Resuscitate Order
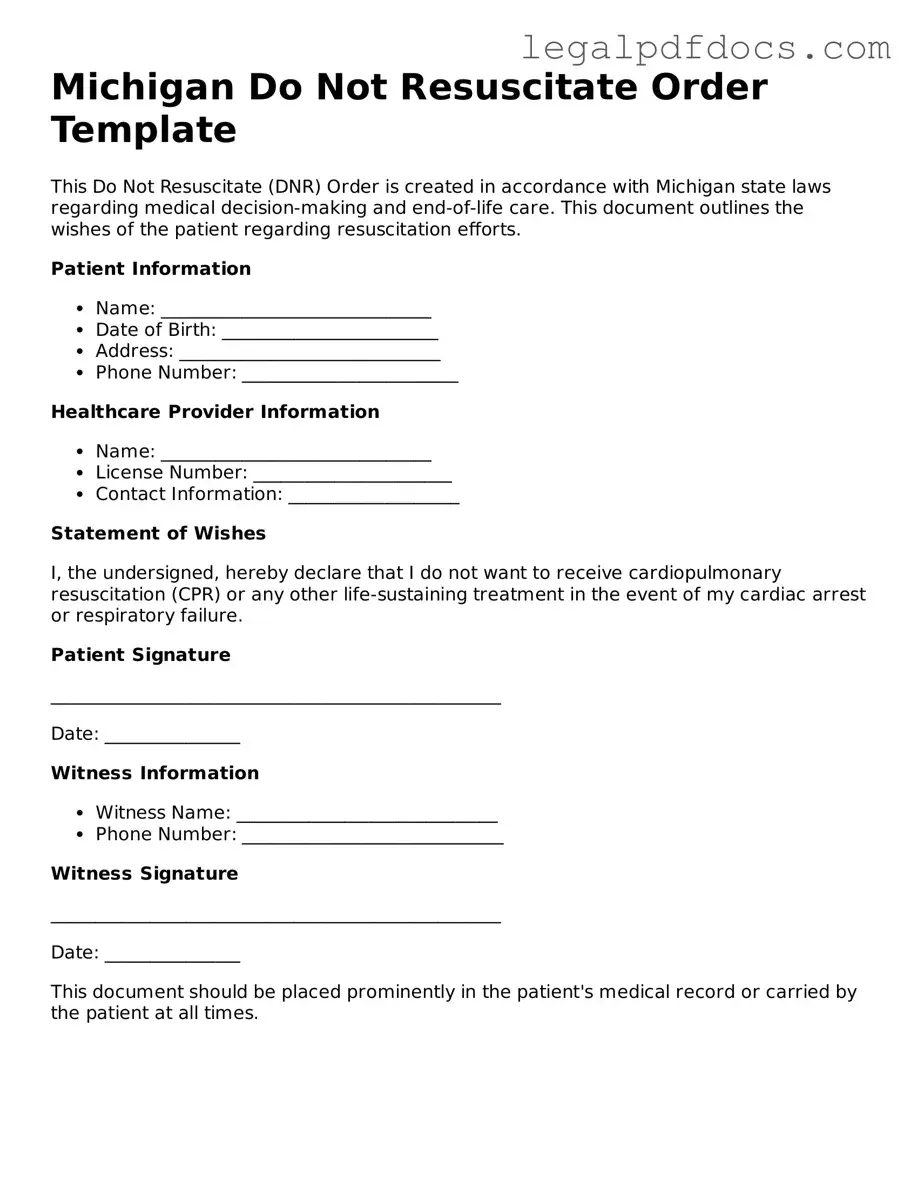
Completing the Michigan Do Not Resuscitate Order form is an important step in expressing your medical care preferences. After filling out the form, it will need to be signed and witnessed according to Michigan law to ensure it is valid. Follow the steps below to accurately complete the form.
- Obtain the Michigan Do Not Resuscitate Order form. This can be found online or through healthcare providers.
- Read the instructions carefully to understand the requirements for filling out the form.
- Provide your full name, date of birth, and address in the designated sections of the form.
- Indicate the name of your physician. This should be a licensed physician who is aware of your wishes.
- Specify the date you are completing the form.
- Sign the form in the designated area to confirm your wishes.
- Have the form witnessed by two individuals who are not related to you and who do not stand to gain from your estate.
- Ensure that a copy of the completed form is kept in a safe place and provided to your healthcare provider and family members.
Find Popular Do Not Resuscitate Order Forms for US States
Dnr Directive - Allows you to communicate your preference against resuscitation efforts.
Whats a Dnr - Understanding the implications of a DNR can lead to more meaningful discussions about end-of-life care.
Illinois Do Not Resuscitate - Family members should be informed about a patient's DNR status to support the decision in a critical situation.
Dnr Form Florida - Individuals with a DNR should wear identification, such as a bracelet, to inform responders.
Documents used along the form
The Michigan Do Not Resuscitate (DNR) Order form is an important document that communicates a patient’s wishes regarding resuscitation efforts in the event of a medical emergency. Several other forms and documents complement the DNR Order, ensuring that patients' healthcare preferences are respected and clearly understood. Below is a list of such documents commonly used in conjunction with the DNR Order in Michigan.
- Advance Directive: This legal document allows individuals to outline their preferences for medical treatment in the event that they become unable to communicate their wishes. It may include instructions about life-sustaining treatments and appoint a healthcare proxy to make decisions on their behalf.
- Durable Power of Attorney for Healthcare: This document designates a specific person to make healthcare decisions for an individual if they are incapacitated. It is crucial for ensuring that a trusted person can advocate for the patient's wishes regarding treatment and care.
- Patient Advocate Designation: Similar to a durable power of attorney, this form allows a patient to appoint a patient advocate who will make healthcare decisions based on the patient’s preferences and values, especially when the patient cannot express their wishes.
- Living Will: A living will is a type of advance directive that specifically addresses the types of medical treatment an individual wishes to receive or forego in the event of a terminal illness or irreversible condition. It provides guidance to healthcare providers and family members.
- Physician Orders for Life-Sustaining Treatment (POLST): This medical order translates a patient’s treatment preferences into actionable medical orders. It is designed for patients with serious illnesses and ensures that their wishes regarding life-sustaining treatments are honored across different healthcare settings.
These documents work together to create a comprehensive approach to advance care planning. By utilizing them alongside the Michigan Do Not Resuscitate Order, individuals can ensure their healthcare preferences are clearly articulated and respected in various medical situations.
Misconceptions
Understanding the Michigan Do Not Resuscitate (DNR) Order form is essential for individuals and families making end-of-life decisions. However, several misconceptions often arise regarding this important document. Here are seven common misconceptions:
-
A DNR order means no medical care will be provided.
This is not true. A DNR order specifically indicates that a person does not want to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. It does not prevent other forms of medical treatment or care.
-
Only terminally ill patients need a DNR.
A DNR order can be appropriate for anyone who wishes to refuse CPR, regardless of their current health status. It is a personal choice and should reflect individual values and wishes.
-
A DNR is only valid in hospitals.
This misconception is incorrect. A DNR order is valid in various settings, including at home, in nursing facilities, and during transport by emergency services, provided that it is properly completed and recognized by medical personnel.
-
Having a DNR order means giving up on life.
Many people view a DNR as a way to maintain dignity and comfort at the end of life. It is a personal decision that reflects an individual's wishes about their care, not a desire to end life prematurely.
-
A DNR order can be verbal.
In Michigan, a DNR order must be documented in writing and signed by a physician. Verbal requests do not hold legal weight and cannot be honored by medical personnel.
-
Once a DNR is signed, it cannot be changed.
This is a misconception. Individuals can revoke or modify their DNR order at any time. It is important to communicate any changes to healthcare providers and ensure that updated documents are readily available.
-
All healthcare providers automatically know about a DNR order.
It is crucial for individuals to ensure that their DNR order is accessible and communicated to all relevant parties, including family members and healthcare providers. Simply having a DNR does not guarantee that it will be recognized without proper communication.
Addressing these misconceptions can help individuals make informed decisions about their healthcare preferences and ensure that their wishes are respected.
PDF Specifications
| Fact Name | Details |
|---|---|
| Purpose | The Michigan Do Not Resuscitate (DNR) Order form is used to indicate a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. |
| Governing Law | This form is governed by the Michigan Public Health Code, specifically under Act 368 of 1978, Section 333.1053. |
| Eligibility | Any adult, or a minor with parental consent, can complete a DNR Order in Michigan if they wish to refuse resuscitation efforts. |
| Signature Requirements | The form must be signed by the patient or their legal representative, and it must also be signed by a physician to be valid. |
| Revocation | A DNR Order can be revoked at any time by the patient or their representative. This can be done verbally or by destroying the form. |
| Distribution | Once completed, copies of the DNR Order should be provided to emergency medical personnel, hospitals, and family members to ensure it is honored. |
Key takeaways
Understanding the Michigan Do Not Resuscitate (DNR) Order form is crucial for ensuring that your healthcare preferences are respected. Here are nine key takeaways:
- Purpose of the DNR: The DNR order informs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest.
- Eligibility: Any adult can complete a DNR order, but it is typically used by individuals with serious health conditions or those who are nearing the end of life.
- Completion: The form must be filled out correctly and signed by the patient or their legal representative to be valid.
- Witness Requirement: A DNR order must be signed by a witness who is not a relative or a healthcare provider involved in the patient's care.
- Healthcare Provider Signature: A physician must sign the DNR order for it to be legally binding. This ensures that the order is recognized in medical settings.
- Communication: It is essential to communicate your DNR wishes to family members and healthcare providers to prevent confusion during emergencies.
- Revocation: You can revoke a DNR order at any time. It is important to inform your healthcare providers and family if you decide to do so.
- Placement: Keep the DNR order in a visible location, such as on the refrigerator or with other important medical documents, to ensure it is easily accessible in emergencies.
- State Compliance: Ensure that the DNR form complies with Michigan state laws, as regulations may vary from state to state.
By understanding these key points, individuals can make informed decisions regarding their end-of-life care and ensure their wishes are honored.