Fill Out a Valid Medication Administration Record Sheet Template
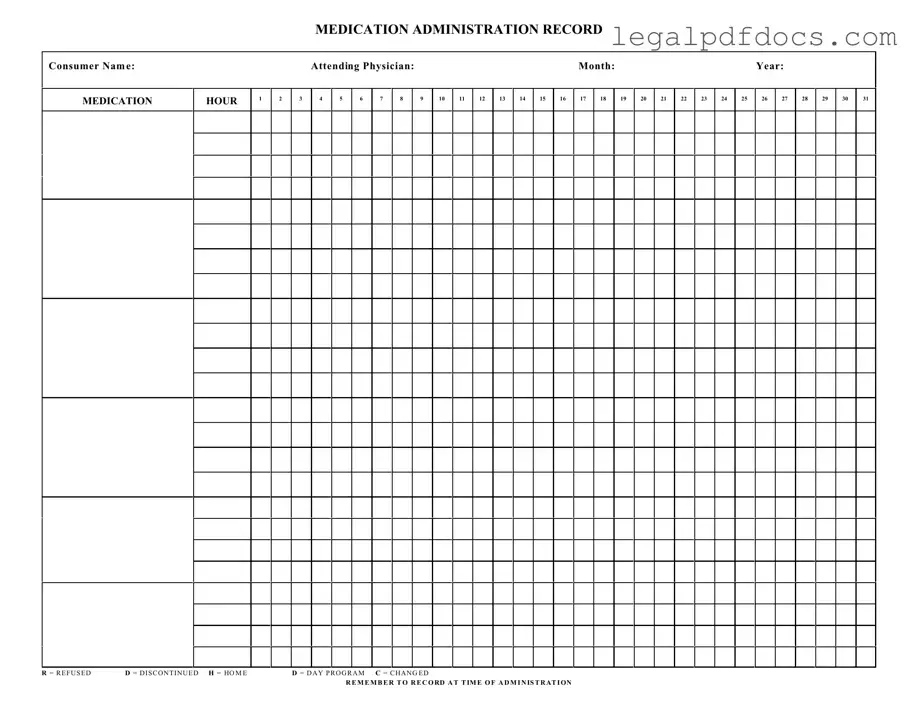
The Medication Administration Record Sheet (MARS) plays a crucial role in the safe and effective administration of medications to consumers. This form is designed to track the administration of prescribed medications, ensuring that each dose is given at the correct time and in the proper manner. It includes essential details such as the consumer's name, the attending physician, and the month and year of administration. The MARS features a grid layout that allows caregivers to document each medication hour, providing a clear visual representation of when medications are administered. Additionally, it includes notations for various situations, such as when a dose is refused, discontinued, or changed, helping to maintain accurate records. Caregivers must remember to record information at the time of administration, which is vital for maintaining a complete and reliable medication history. By using the MARS, healthcare providers can enhance patient safety and ensure compliance with medication protocols.
Dos and Don'ts
When filling out the Medication Administration Record Sheet form, there are important practices to follow to ensure accuracy and compliance. Here are four things to do and not to do:
- Do: Clearly write the consumer's name at the top of the form.
- Do: Record the medication administration time accurately for each dose.
- Do: Use the appropriate codes for refusal, discontinued, or changed medications.
- Do: Ensure the attending physician's name is included for reference.
- Don't: Leave any sections blank; incomplete forms can lead to errors.
- Don't: Use abbreviations that are not standard or widely understood.
- Don't: Forget to document any changes or refusals at the time of administration.
- Don't: Alter the form after it has been filled out; changes should be made on a new form.
How to Use Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is essential for tracking medication administration accurately. Follow these steps to ensure that all necessary information is recorded properly.
- Enter Consumer Name: Write the full name of the individual receiving the medication at the top of the form.
- Fill in Attending Physician: Provide the name of the physician responsible for the consumer’s care.
- Specify Month and Year: Indicate the month and year for which the medication is being administered.
- Record Medication Hours: Mark the appropriate hour(s) when the medication is administered, using the designated columns for each hour.
- Document Medication Status: Use the provided codes to indicate the status of the medication, such as R for Refused, D for Discontinued, H for Home, D for Day Program, and C for Changed.
- Note the Date: Ensure that the date of administration is clearly recorded next to the corresponding medication hour.
- Review for Accuracy: Double-check all entries for correctness before finalizing the record.
More PDF Templates
Dating Application Form Funny - Meet your new partner in love and fun.
Erc Forms - Necessary information such as homeowner contact details and property address should be included.
Documents used along the form
The Medication Administration Record Sheet is a crucial document used in healthcare settings to track the administration of medications to patients. Alongside this form, several other documents are often utilized to ensure comprehensive medication management and patient safety. Below is a list of related forms and documents that support the medication administration process.
- Medication Order Form: This document outlines the specific medications prescribed by a physician, including dosage, frequency, and route of administration. It serves as the primary source for medication information.
- Patient Medication Profile: This profile contains a comprehensive list of all medications a patient is currently taking, including over-the-counter drugs and supplements. It helps healthcare providers avoid potential drug interactions.
- Medication Reconciliation Form: This form is used to compare a patient's current medication list with newly prescribed medications. It ensures continuity of care and reduces the risk of errors during transitions between care settings.
- Incident Report Form: In cases where a medication error occurs, this document is completed to detail the event, including what happened, when, and any actions taken. It is essential for quality assurance and improving practices.
- Patient Education Record: This record documents the information provided to patients regarding their medications, including potential side effects and instructions for use. It supports patient understanding and adherence to treatment.
- Controlled Substance Log: For medications classified as controlled substances, this log tracks the dispensing and administration of these drugs. It is vital for compliance with regulatory requirements.
- Allergy and Adverse Reaction Record: This document lists any known allergies or adverse reactions a patient has experienced. It is critical for preventing allergic responses during medication administration.
- Medication Administration Policy Manual: This manual outlines the procedures and protocols for medication administration within a healthcare facility. It serves as a reference for staff to ensure adherence to best practices.
These documents collectively enhance the safety and effectiveness of medication administration, ensuring that healthcare providers have the necessary information to make informed decisions about patient care. Proper use of these forms promotes accountability and supports optimal health outcomes for patients.
Misconceptions
Understanding the Medication Administration Record Sheet is crucial for proper medication management. However, several misconceptions can lead to confusion. Here are six common misunderstandings:
- It's only for nurses. Many people think that only nurses can fill out this form. In reality, anyone responsible for administering medication, including caregivers and family members, can use it.
- It's optional. Some believe that using the Medication Administration Record Sheet is optional. In fact, it is a vital tool for ensuring accurate medication tracking and accountability.
- It doesn't need to be updated. A common myth is that once the form is filled out, it doesn't require further updates. Regular updates are necessary to reflect any changes in medication or dosage.
- All medications are listed on the form. People often assume that every medication will be pre-printed on the form. However, it is essential to manually enter new medications as they are prescribed.
- Recording is only necessary at the time of administration. Some believe that notes should only be made during medication administration. It's important to document any changes or refusals as soon as they occur.
- It's the same as a prescription pad. Many confuse the Medication Administration Record Sheet with a prescription pad. While both are related to medication, the record sheet is specifically for tracking administration, not prescribing.
By clearing up these misconceptions, individuals can better utilize the Medication Administration Record Sheet, ensuring safe and effective medication management.
File Specs
| Fact Name | Details |
|---|---|
| Purpose | The Medication Administration Record (MAR) sheet is used to document the administration of medications to patients. |
| Consumer Information | The form includes a section for the consumer's name, ensuring accurate identification of the patient receiving medication. |
| Physician Details | It requires the name of the attending physician, which helps maintain a clear line of communication regarding patient care. |
| Monthly Tracking | The MAR sheet is organized by month and includes space for each day, allowing for comprehensive tracking of medication administration. |
| Hour Tracking | It provides designated hours for medication administration, ensuring that doses are given at the correct times. |
| Abbreviations | The form includes specific abbreviations such as R (Refused), D (Discontinued), and H (Home), which streamline the documentation process. |
| State Regulations | In many states, the use of a MAR sheet is governed by laws related to medication administration in healthcare settings, such as the Nurse Practice Act. |
Key takeaways
When using the Medication Administration Record Sheet, it’s essential to follow a few key guidelines to ensure accuracy and safety in medication administration. Here are some important takeaways:
- Complete Consumer Information: Always fill in the consumer's name, attending physician, month, and year at the top of the form. This helps in identifying the individual and tracking their medication history.
- Record Administration Times: Clearly mark the hour when medication is administered. This helps maintain a consistent schedule and ensures that doses are given on time.
- Use Correct Codes: Familiarize yourself with the codes for recording medication status, such as R for Refused, D for Discontinued, H for Home, and C for Changed. This standardization aids in clear communication.
- Document Refusals: If a consumer refuses medication, it is crucial to record this immediately. This ensures that all parties are aware of the situation and can respond appropriately.
- Update Changes Promptly: If there are any changes in the medication regimen, document them as soon as they occur. This helps in maintaining accurate records and avoiding confusion.
- Review Daily: Regularly review the Medication Administration Record Sheet to ensure all entries are complete and accurate. This helps catch any potential errors early.
- Maintain Confidentiality: Keep the record secure and private. Protecting consumer information is not only ethical but also a legal requirement.
- Communicate with the Team: Share any concerns or observations about the consumer's response to medication with the healthcare team. Open communication is vital for effective care.
By adhering to these guidelines, you can help ensure that the medication administration process is safe and effective for all consumers.