Fill Out a Valid Cna Shower Sheets Template
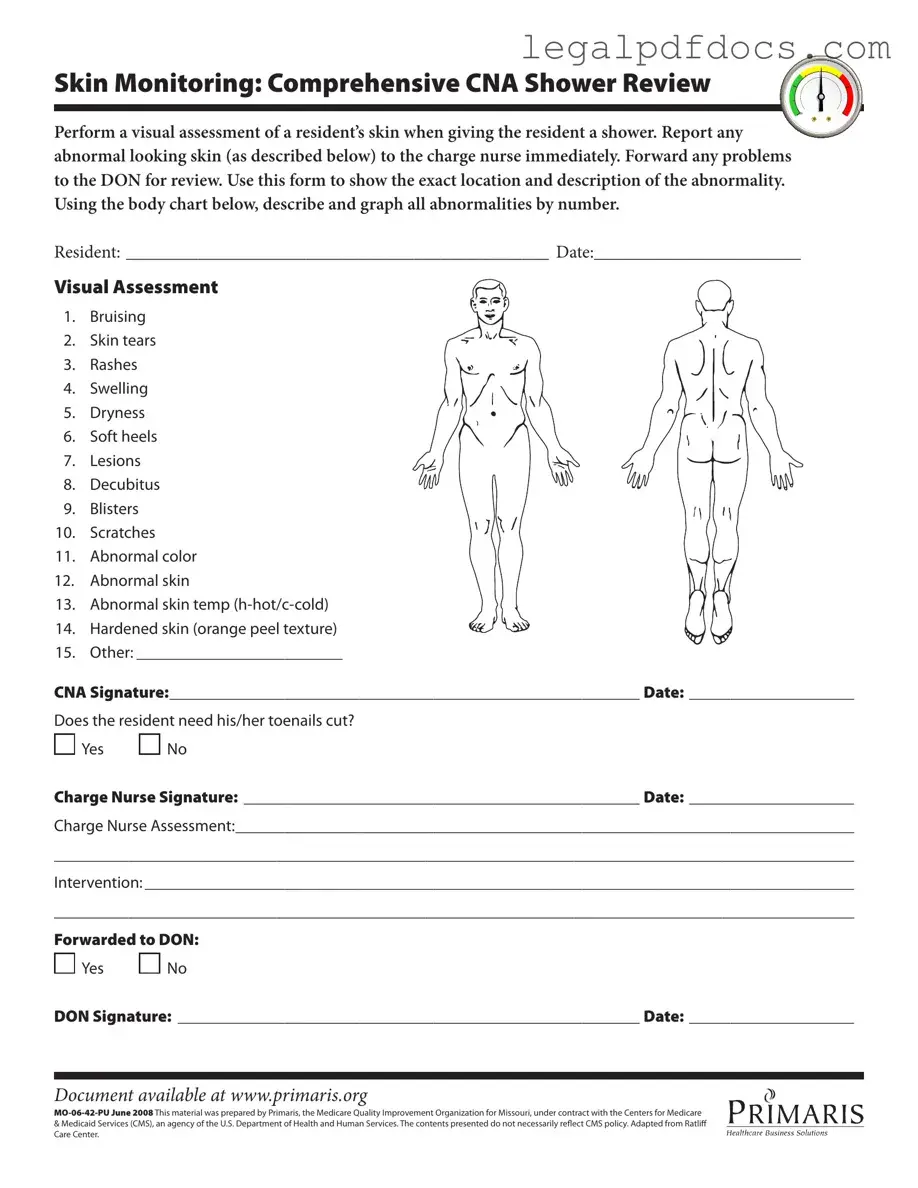
The CNA Shower Sheets form plays a crucial role in ensuring the health and well-being of residents in care facilities. This form is primarily designed for Certified Nursing Assistants (CNAs) to conduct thorough skin assessments during showering. As part of their routine, CNAs visually inspect residents' skin for various abnormalities, such as bruising, rashes, and skin tears. Immediate reporting of any concerning findings to the charge nurse is essential, allowing for timely intervention and care. The form includes a detailed body chart where CNAs can accurately document the location and description of any skin issues observed. It also prompts CNAs to assess the condition of toenails, which can significantly impact a resident's comfort and mobility. The charge nurse is then required to evaluate the CNA's findings, and if necessary, further actions can be escalated to the Director of Nursing (DON). This systematic approach not only helps in maintaining skin integrity but also fosters a collaborative environment among the caregiving team, ultimately enhancing the quality of care provided to residents.
Dos and Don'ts
When filling out the CNA Shower Sheets form, it is crucial to ensure accuracy and clarity. Here are five important dos and don'ts to consider:
- Do perform a thorough visual assessment of the resident's skin during the shower.
- Do report any abnormalities, such as bruising or rashes, to the charge nurse immediately.
- Do use the body chart provided to accurately describe and graph all abnormalities.
- Do ensure your signature and date are clearly written at the bottom of the form.
- Do forward any issues to the Director of Nursing (DON) for further review.
- Don't leave any sections of the form blank, as this could lead to miscommunication.
- Don't use vague descriptions when noting abnormalities; be specific.
- Don't forget to check if the resident needs toenail care and indicate it on the form.
- Don't delay reporting any serious skin issues; timely action is essential.
- Don't neglect to review the completed form for errors before submission.
How to Use Cna Shower Sheets
To complete the CNA Shower Sheets form effectively, follow these steps carefully. This will ensure that all necessary information is accurately documented for the resident's care. Make sure to gather all relevant details before starting the process.
- Begin by filling in the resident's name in the RESIDENT section.
- Enter the date of the assessment in the DATE field.
- Conduct a visual assessment of the resident's skin while giving the shower.
- Identify any abnormalities from the provided list, such as bruising, rashes, or skin tears.
- Use the body chart to graphically represent the location of any abnormalities by number.
- In the Other section, specify any additional findings that are not listed.
- Sign and date the form in the CNA Signature section.
- Indicate whether the resident needs toenail trimming by selecting Yes or No.
- Have the charge nurse sign and date the Charge Nurse Signature section after reviewing the assessment.
- Document the charge nurse's assessment in the designated area.
- Outline any interventions that will be taken based on the findings in the Intervention section.
- Mark whether the report has been forwarded to the Director of Nursing (DON) by selecting Yes or No.
- If forwarded, ensure the DON signs and dates the DON Signature section.
More PDF Templates
P 45 Meaning - The form includes sections for gender and date of birth for demographic records.
Stock Ledger - Captures the certificate number of any surrendered shares.
Broker Price Opinion Sample - The report aims to provide a clear roadmap for property evaluation and marketing strategy.
Documents used along the form
The CNA Shower Sheets form is an essential tool for documenting the condition of residents' skin during showers. However, it is often accompanied by several other forms and documents that support comprehensive care and record-keeping. Below is a list of commonly used forms that work in conjunction with the CNA Shower Sheets.
- Incident Report: This document is used to record any unusual occurrences or accidents involving residents. It details the nature of the incident, the individuals involved, and any immediate actions taken.
- Daily Care Log: Caregivers fill out this log to document the daily activities and health status of residents. It includes notes on meals, medications, and any significant changes in behavior or condition.
- Skin Assessment Form: This form provides a more detailed evaluation of a resident's skin condition. It may include specific criteria for assessing different types of skin issues and tracking changes over time.
- Care Plan: The care plan outlines the specific needs and goals for each resident. It includes interventions and strategies to address any identified issues, ensuring a tailored approach to care.
- Medication Administration Record (MAR): This record tracks the medications administered to residents. It includes information on dosages, times, and any reactions observed, helping to ensure safe medication practices.
- Vital Signs Record: This document is used to log the vital signs of residents, such as blood pressure, heart rate, and temperature. Monitoring these signs is crucial for assessing overall health and detecting potential issues early.
- Referral Form: When a resident requires additional services or specialist evaluations, a referral form is completed. This document facilitates communication with other healthcare providers and ensures continuity of care.
- Family Communication Log: This log documents interactions with residents' family members. It includes updates on the resident's condition, care plans, and any concerns raised by family members.
- Discharge Summary: When a resident is discharged from care, this summary provides a comprehensive overview of their treatment, progress, and any follow-up recommendations, ensuring a smooth transition to the next stage of care.
These documents collectively enhance the quality of care provided to residents and ensure that all aspects of their health and well-being are thoroughly documented and communicated among the care team. Proper use of these forms supports effective monitoring, intervention, and overall resident safety.
Misconceptions
Misconceptions about the CNA Shower Sheets form can lead to misunderstandings regarding its purpose and use. Here are ten common misconceptions along with clarifications:
- The form is only for documenting serious skin issues. Many believe that the form is only necessary for severe conditions. In reality, it is designed to document all types of skin abnormalities, regardless of severity.
- Only the CNA can fill out the form. Some think that only Certified Nursing Assistants (CNAs) are allowed to complete the form. However, it is a collaborative tool that may involve input from other healthcare staff.
- The form is optional. There is a misconception that using the form is optional. In fact, it is a required part of the skin monitoring process to ensure residents receive appropriate care.
- Documentation is only necessary if there is a visible problem. Many believe that documentation is only needed for visible issues. However, the form encourages thorough assessments, even if problems are not immediately visible.
- Skin assessments are only needed during showers. Some individuals think that skin assessments should only occur during showers. Regular monitoring is essential, and assessments should be made at various times, not just during bathing.
- The form is solely for the CNA's use. There is a belief that the form is only for the CNA's reference. In reality, it serves as a communication tool among the entire healthcare team, including nurses and the Director of Nursing (DON).
- All abnormalities must be reported immediately. Some think that every minor finding must be reported right away. While significant issues should be reported immediately, minor findings can be documented and monitored.
- The form does not require a signature. It is a common misconception that the form does not need signatures. Both the CNA and the charge nurse must sign it to validate the assessment and interventions.
- Only skin issues are documented. Some assume that the form is limited to skin problems. It also includes other relevant assessments, such as toenail care needs, which are important for overall resident health.
- The form is outdated and not relevant. There may be a belief that the form is no longer applicable. However, it is regularly updated to reflect current best practices in resident care.
File Specs
| Fact Name | Details |
|---|---|
| Purpose of the Form | The CNA Shower Sheets form is designed to document skin assessments during resident showers, ensuring any abnormalities are reported to nursing staff promptly. |
| Skin Abnormalities | The form includes a comprehensive list of skin conditions to monitor, such as bruising, rashes, and decubitus, allowing for detailed tracking and intervention. |
| Signature Requirements | Both the CNA and charge nurse must sign the form, ensuring accountability and proper communication regarding the resident's skin condition. |
| Governing Law | This form is governed by state regulations related to nursing home care and patient safety, particularly in Missouri, under the oversight of CMS. |
Key takeaways
When using the CNA Shower Sheets form, it is important to understand its purpose and how to fill it out effectively. Here are key takeaways to keep in mind:
- Visual Assessment is Critical: Conduct a thorough visual assessment of the resident's skin during the shower. This helps identify any issues early.
- Immediate Reporting: If any abnormal skin conditions are observed, report them to the charge nurse without delay.
- Document Abnormalities: Use the form to accurately document the location and description of any skin abnormalities.
- Body Chart Usage: Utilize the body chart provided on the form to graphically indicate the areas of concern.
- Comprehensive List of Conditions: Be familiar with the list of conditions to monitor, including bruising, rashes, and decubitus.
- Toenail Care: Assess whether the resident needs toenail trimming and indicate your findings on the form.
- Charge Nurse Assessment: Ensure that the charge nurse reviews the form and adds their assessment to provide continuity of care.
- Forwarding to DON: If necessary, forward the completed form to the Director of Nursing (DON) for further evaluation and intervention.
By following these takeaways, you can ensure that the CNA Shower Sheets form is filled out accurately and effectively, promoting better skin health for residents.