Fill Out a Valid Advance Beneficiary Notice of Non-coverage Template
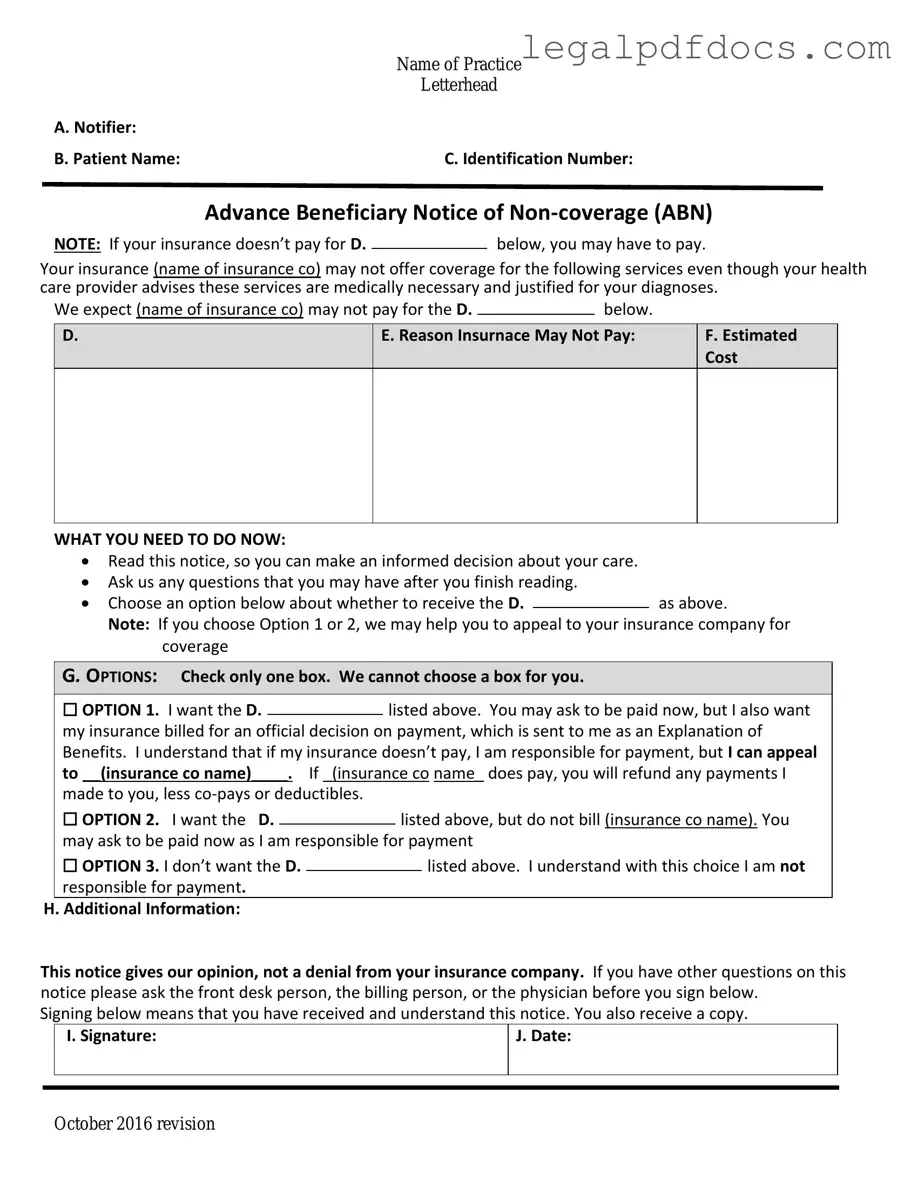
The Advance Beneficiary Notice of Non-coverage, commonly referred to as the ABN, plays a crucial role in the Medicare system by informing beneficiaries about services that may not be covered by their health insurance. This form serves as a notification to patients that certain medical services or items may not be reimbursed by Medicare, allowing individuals to make informed decisions regarding their care. It outlines the specific reasons why a service might be denied coverage, which can include factors such as the service being deemed unnecessary or not meeting Medicare’s coverage criteria. Additionally, the ABN provides beneficiaries with the opportunity to accept or decline the service, thus promoting transparency and empowering patients to take charge of their healthcare choices. By signing the ABN, patients acknowledge their understanding of the potential financial responsibility they may incur if they choose to proceed with the service. The form is not only a protective measure for healthcare providers, shielding them from liability regarding payment disputes, but it also fosters clear communication between providers and patients, ultimately enhancing the overall healthcare experience. Understanding the nuances of the ABN is essential for both beneficiaries and providers, as it can significantly impact the delivery and financing of medical care.
Dos and Don'ts
When filling out the Advance Beneficiary Notice of Non-coverage form, it is important to follow certain guidelines to ensure accuracy and compliance. Below is a list of things you should and shouldn't do.
- Do read the instructions carefully before starting the form.
- Do provide accurate information regarding your medical services.
- Do sign and date the form to confirm your understanding.
- Do keep a copy of the completed form for your records.
- Do ask questions if you are unsure about any part of the form.
- Don't leave any required fields blank.
- Don't use incorrect or outdated information.
- Don't ignore the deadlines for submission.
- Don't forget to check for any additional documentation that may be required.
- Don't hesitate to seek assistance if needed.
How to Use Advance Beneficiary Notice of Non-coverage
Once you have the Advance Beneficiary Notice of Non-coverage form, you will need to fill it out carefully. This process ensures that you provide all necessary information for your healthcare provider and Medicare. Follow these steps to complete the form accurately.
- Start by entering the patient's name at the top of the form. Make sure to spell it correctly.
- Fill in the patient's Medicare number. This number is essential for identification purposes.
- Provide the date of service. Write the exact date when the service was provided.
- In the next section, describe the service or item that is being discussed. Be clear and specific.
- Indicate the reason why you believe the service may not be covered. This could be due to a variety of factors, so be honest.
- Sign and date the form at the bottom. Your signature confirms that you understand the information provided.
- Make a copy of the completed form for your records before submitting it.
After filling out the form, submit it to your healthcare provider. They will review the information and guide you on the next steps. Keep an eye on any correspondence you receive regarding coverage decisions.
More PDF Templates
Is Certificate of Live Birth the Same as Birth Certificate - The certificate must be filed promptly following the birth, usually within days.
Faa Form 8050-2 - Proper documentation with the Aircraft Bill of Sale supports aircraft valuation assessments.
Documents used along the form
The Advance Beneficiary Notice of Non-coverage (ABN) is an important document used in healthcare settings to inform patients that certain services may not be covered by Medicare. Alongside the ABN, several other forms and documents are commonly utilized to ensure clear communication between healthcare providers and patients regarding coverage and billing. Below is a list of these documents, each serving a specific purpose.
- Medicare Claim Form (CMS-1500): This form is used by healthcare providers to bill Medicare for services rendered. It provides detailed information about the patient, the services provided, and the costs involved.
- Notice of Exclusion from Medicare Benefits (NEMB): This document is issued when a service is not covered by Medicare. It explains the reasons for non-coverage and informs patients about their financial responsibilities for the service.
- Patient Authorization Form: This form allows healthcare providers to obtain consent from patients to share their medical information with third parties, such as insurance companies. It ensures that patient privacy is maintained while facilitating necessary communication for billing purposes.
- Medicare Summary Notice (MSN): The MSN is a document that Medicare beneficiaries receive, summarizing the services billed to Medicare. It outlines what was covered, what was not covered, and any amounts the patient may owe.
Understanding these documents can help patients navigate their healthcare experiences more effectively. Each form plays a crucial role in ensuring transparency and clarity regarding coverage, billing, and patient rights. Being informed about these documents can empower patients to make better decisions about their healthcare options.
Misconceptions
The Advance Beneficiary Notice of Non-coverage (ABN) form can often be misunderstood. Here are six common misconceptions about this important document:
-
The ABN is only for Medicare patients.
This is incorrect. While the ABN is primarily associated with Medicare, it can also be used in other healthcare settings where patients may need to be informed about potential non-coverage of services.
-
Receiving an ABN means the service will definitely not be covered.
This is misleading. An ABN indicates that the provider believes a service may not be covered, but it does not guarantee that coverage will be denied. Coverage decisions are made by Medicare or the insurance provider.
-
Patients must pay for services if they receive an ABN.
Not necessarily. The ABN gives patients the option to accept or refuse the service. If they choose to proceed, they may be responsible for payment if the service is ultimately deemed non-covered.
-
All healthcare providers are required to issue an ABN.
This is not true. Only providers who participate in Medicare and anticipate that a service may not be covered must issue an ABN. Not all services require this notice.
-
The ABN is a legally binding contract.
This misconception can lead to confusion. The ABN is not a contract; rather, it is a notification that informs patients about potential non-coverage and their financial responsibilities.
-
Signing an ABN means you agree to pay for the service.
This is incorrect. Signing the ABN indicates that you understand the potential for non-coverage, but it does not obligate you to pay if you later decide not to proceed with the service.
Understanding these misconceptions can help patients navigate their healthcare options more effectively and make informed decisions regarding their services and potential costs.
File Specs
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service may not be covered. |
| When to Use | Providers must issue an ABN when they believe that Medicare might deny payment for a service or item. |
| Beneficiary Rights | Beneficiaries have the right to receive the ABN before the service is provided, allowing them to make informed decisions. |
| Signature Requirement | Beneficiaries must sign the ABN to acknowledge understanding that they may be responsible for payment if Medicare denies coverage. |
| State-Specific Forms | Some states may have additional requirements or specific forms that align with local laws governing healthcare services. |
| Validity Period | The ABN is valid for the specific service or item listed and should be issued for each instance where coverage is uncertain. |
| Consequences of Not Issuing | If an ABN is not provided, the provider may not be able to collect payment from the beneficiary for non-covered services. |
| Governing Laws | Medicare guidelines govern the use of ABNs, with specific state laws potentially influencing the process in certain jurisdictions. |
Key takeaways
- Understand the Purpose: The Advance Beneficiary Notice of Non-coverage (ABN) form informs patients that Medicare may not cover a specific service or item.
- Timing is Crucial: Fill out the ABN before receiving the service. This ensures you are aware of potential costs upfront.
- Read Carefully: Review the form closely. It outlines the service, the reason for non-coverage, and your financial responsibilities.
- Make Informed Decisions: The ABN allows you to decide whether to proceed with the service despite the possibility of non-coverage.
- Keep a Copy: Retain a copy of the signed ABN for your records. This can be important if there are disputes about coverage later.
- Ask Questions: If you do not understand any part of the ABN, ask the healthcare provider for clarification before signing.
- Know Your Rights: You have the right to refuse the service if you disagree with the non-coverage notice. Understand the implications of your choice.